CMPA and lactose intolerance in infants
Lactose intolerance, common in adults, is less frequent in infants. Lactose intolerance is rare at this age, but since infants feed exclusively on milk in the first few months of their lives, it is important to detect it. Lactose intolerance is sometimes confused with cow’s milk protein allergy (CMPA). It is therefore important to know the difference between CMPA and lactose intolerance in infants, in order to adapt their diet correctly.
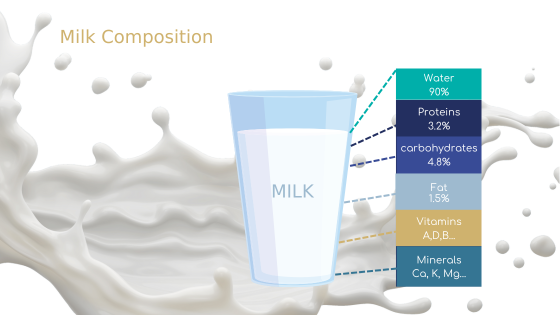
Milk composition
Milk is the mainstay of infant nutrition in all mammals. Its varied composition of different nutrients ensures the healthy development of the newborn. Cow’s milk contains nutrients such as carbohydrates (4.8%), proteins (3.2%), lipids (1.5%), vitamins (A, D, B, etc.) and minerals (calcium, potassium, etc.). [1]
Milk proteins, potential allergens [2]
Proteins are the second main component of milk. It contains between 3 and 3.5 g of protein per 100 mL, 80% of which is casein and 20% soluble protein.
Milk proteins include over 20 allergens, including α-lactalbumin, β-lactoglobulin, immunoglobulins and serum albumin. Most children are sensitive to more than one protein.
Milk sugar: lactose
Lactose is the sugar naturally present in milk. Cow’s milk contains 5g per 100 mL of lactose. By way of comparison, for the same volume, breast milk contains 7.5g of lactose.[3]
Lactose is a very important compound, as it contributes to a large proportion of an infant’s total daily energy.
Milk proteins allergies
Cow’s milk is a widely consumed food, used as a base for infant formula. In Europe, between 0.5% and 4.9% of babies suffer from CMPA.[4]
CMPA: the most common allergy in infants [3]
An allergy is an overreaction of the immune system to a foreign substance called an allergen. To limit allergy-induced symptoms, the solution is to avoid all contact with the allergen.
Cow’s milk protein allergy, or CMPA, is the most common allergy in infants. It generally appears during the first 2 years of a child’s life.
CMPA is a reproducible adverse reaction to one or more cow’s milk proteins. Like other food allergies, CMPA can be:
- Immunoglobulin E (IgE)-mediated,
- Non-IgE-mediated,
- Mediated and non-mediated.
Symptoms and consequences of CMPA [3]
Reactions depend on the type of allergy. If it is IgE-mediated, the allergy leads to skin reactions, facial swelling and severe allergic reactions such as anaphylaxis. In the case of a non-IgE-mediated allergy, the infant may suffer from vomiting, diarrhea, feeding difficulties, sleep problems and stunted growth. Other symptoms may include inflammation of the esophagus, eczema and respiratory problems.
Diagnosis of CMPA [3]
Detection of this disease is necessary to avoid an unnecessary avoidance diet. Diagnosis must therefore be made as soon as signs and symptoms appear. It can be made using a variety of tests, such as a clinical history, physical examination, specific IgE allergy tests, skin tests, and sometimes oral provocation tests.
What strategies should be implemented? [3]
In the case of a non-breast-fed infant, the first solution is strict avoidance of cow’s milk protein. This means replacing it with a formula based on highly hydrolyzed cow’s milk protein or rice protein hydrolysate.

Lactose intolerance
Lactose intolerance is the inability of the digestive system to fully digest lactose. Some intolerances are temporary, following infection by a pathogen, for example, but some are lifelong. These usually occur as we age.
Lactose intolerance in adults is due to an inherited genetic anomaly called primary lactase deficiency, but in infants the causes are different.
Lactose metabolism: the cause of intolerance
Lactose requires enzymatic hydrolysis by the lactase present in the digestive tract. This breaks the glycosidic bond, releasing D-glucose and D-galactose, which are then absorbed in the small intestine.
In the case of lactase failure, poorly absorbed lactose ends up in the colon, where it is metabolized by bacteria. The bacteria use the sugar as a nutrient, producing short-chain fatty acids, methane, dihydrogen, carbon dioxide or lactic acid.[5]
4 types of lactose intolerance in infants [6]
Infants have enough lactase to digest one liter of breast milk a day (i.e., 60 to 70 g of lactose). In fact, enzymatic activity peaks at birth, then diminishes around the age of 1 or 2, depending on milk consumption. In some children, lactase activity disappears completely, causing lactose intolerance. However, in young children, intolerance is caused by underlying intestinal pathologies.[5]
There are 4 causes of lactose intolerance in young children.
Firstly, in premature infants, the enterocytes that develop during the third trimester of pregnancy are not functional. It is these cells, lining the intestinal wall, which produce lactase. As a result, these infants are deprived of lactase and are therefore transiently lactose intolerant. As the child’s digestive system matures, lactase activity is restored.
Secondly, the cause may be hereditary. This very rare anomaly may result from a congenital lactase deficiency due to a mutation in the gene responsible for synthesizing the enzyme.
The third type of intolerance concerns only older children: primary intolerance. It is caused by an early decrease in lactase expression. This is the most frequent type in these children.
Finally, secondary intolerance is an intolerance engendered by a pathology that damages the small intestine and thus the mature lactase-producing enterocytes. In most cases, secondary intolerance is reversible. In fact, once the pathology has been treated and the intestinal mucosa repaired, lactose can once again be digested by the infant. The most common example in children is gastroenteritis.
Lactose intolerance in children under 5 is very rare. It is usually transitory and disappears with treatment of the pathology causing it.
Symptoms and consequences of lactose intolerance [5]
Clinical manifestations are mainly digestive. They appear a few hours after ingestion of products containing lactose. They include abdominal pain, flatulence, bloating, nausea and vomiting. Symptoms vary widely, depending on the child and the amount of lactose ingested.
Adapting consumption to limit symptoms [5]
When avoiding dairy products, whether temporarily or not, dietary monitoring is essential to avoid nutritional deficiencies. Dairy products are rich in vitamins B2, vitamin D and calcium, all essential micronutrients for healthy infant development. Regarding secondary intolerances, the reintroduction of foods containing lactose can be attempted 2 to 4 weeks after the end of the pathology.
As a rule, foods containing lactose should not be totally excluded. It is quite possible to give them to the child in small, divided doses during a meal, which slows down the release of lactose in the small intestine.

APLV and lactose intolerance: two disorders to be clearly differentiated
CMPA and lactose intolerance in infants: similar symptoms
What makes diagnosis so complicated is the similarity between certain symptoms. In fact, both disorders induce digestive problems such as bloating, stomachache, abdominal cramps, gurgling, nausea and/or diarrhea.
CMPA and lactose intolerance in infants: two very different disorders
Firstly, CMPA involves the immune system. Certain symptoms are therefore characteristic of an allergy, such as itchy skin rashes, wheezing, runny nose and cough. These symptoms are totally absent in lactose intolerance.[5]
Finally, the similarity of certain symptoms and the difference in treatments make it even more important to differentiate the two disorders. Indeed, the wrong treatment or unnecessary avoidance of lactose can lead to unnecessary deficiencies in the nutrients essential for the proper development of infants.6 It is therefore vital to make a precise diagnosis and adapt the child’s diet accordingly.
At Lactalis Ingredients, we offer low-lactose products with a protein composition capable of providing a good supply of amino acids. In fact, Prolacta® is developed using a process that preserves the nutritional and functional properties of proteins, while ensuring a lower total protein content in infant formulas. Incorporating this ingredient into infant formulas therefore contributes to the growth and healthy development of lactose-intolerant infants. Nevertheless, due to its composition of cow’s milk proteins, Prolacta® cannot be used in its current state for children suffering from CMPA.
Any question ? Contact-us !
Sources:
[1] Institut professionnel du lait de consommation, La composition du lait
[2] A.Giannetti, Cow’s milk protein allergy as a model of food allergies, Published online 2021 Apr 30. doi: 10.3390/nu13051525, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8147250/
[3] R.G.Heine, Lactose intolerance and gastrointestinal cow’s milk allergy in infants and children -common misconceptions reviseited, Published online 2017 Dec 12. doi: 10.1186/s40413-017-0173-0
[4] Vandenplas Y, Broekaert I, Domellöf M, Indrio F, Lapillonne A, Pienar C, et al. An ESPGHAN position paper on the diagnosis, management and prevention of cow’s milk allergy. J Pediatr Gastroenterol Nutr. 26 juill 2023
[5] F.Fassio, Lactose Maldigestion, Malabsorption, and Intolerance: A Comprehensive Review with a Focus on Current Management and Future Perspectives, 2018
[6] National Institute of Diabetes and digestive and kidney diseases